 BBC
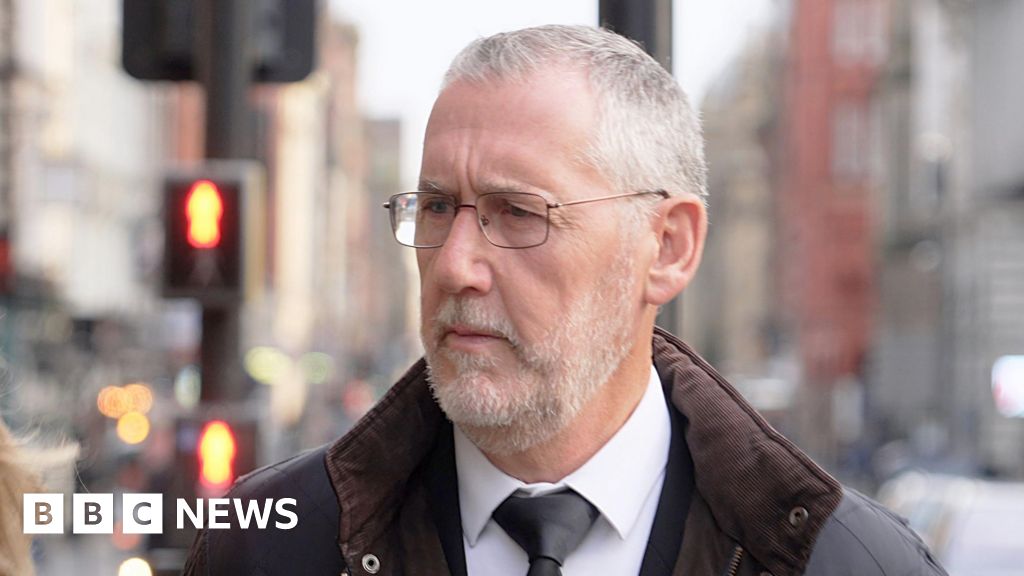
BBCThe former medical director of the hospital where Lucy Letby murdered babies has apologised to consultants “if they felt intimidated” by him.
Ian Harvey was the most senior doctor at the Countess of Chester Hospital when the nurse killed seven infants and tried to take the lives of seven others between 2015 and 2016.
Giving evidence for a second day at the public inquiry into the circumstances of the crimes, he said one of the greatest regrets of his career was the breakdown in relationships between the hospital’s executives and consultants.
Mr Harvey accepted he failed in his duty of pastoral care to the paediatricians who were trying to raise the alarm about Letby, who they had noted was often present when babies died or came close to death suddenly and unexpectedly.
But he denied threatening the doctors with referral the General Medical Council regulator, adding that this had been a threat made instead by Lucy Letby’s father John.
 Cheshire Police
Cheshire PoliceRachel Langdale KC, counsel to the inquiry, asked Mr Harvey if he had sought permission from the victims’ parents for their children’s medical records to be used in a case note review of some of the unexpected deaths at the neonatal unit.
Mr Harvey said he could not recall whether he had done this but, when pressed by Ms Langdale, he said: “I almost certainly would have delegated that task.
“I have no recollection of following that through. If I didn’t, that is a very significant error on my part and I’m very sorry for that.”
Mr Harvey was also asked why he went ahead with a review of the neonatal unit by the Royal College of Paediatrics and Child Health when the reviewers had told him they could not directly address the cause of the rise in unexpected deaths and collapses.
Ms Langdale said: “You were spending money and taking time on a review that isn’t going to answer the question you’ve got in front of you [that consultants paediatricians were concerned that Letby was deliberately harming babies]?”
Mr Harvey replied: “It was perfectly reasonable to explore with the relevant expertise, both medical and nursing, the full range of potential causes.”
 EPA
EPAHe was also asked why he told a hospital committee that the Royal College did not recommend any immediate action in respect of the increased mortality, when it had actually recommended the hospital start its own investigation into the doctors’ concerns.
Mr Harvey replied that he did not think it was an immediate concern where The Royal College “say you have to take action before we leave the building or stop this service now”.
Ms Langdale put it to Mr Harvey that, under his tenure as medical director, doctors were afraid they would lose their jobs for raising patient safety concerns.
He responded: “I accept I failed in a duty of pastoral care that I should have offered.”
But he said he did not seek to create a climate of fear on the unit.
He also denied telling Susan Gilbey, who took over as chief executive at the hospital, that she should refer consultants to the General Medical Council.
“I did not say that,” he said.
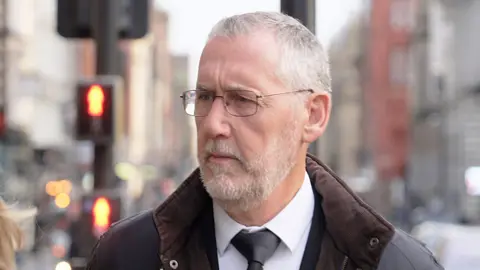
The Thirlwall inquiry, held at Liverpool Town Hall, continues.
 Reuters
Reuters