

Recent data from the Household Pulse Survey (2022 to 2023) indicates that, of the millions of Americans previously infected with COVID-19, more than 7% developed post-acute sequelae of COVID-19 (PASC). Otherwise known as long COVID, PASC refers to a syndrome entailing multisystem dysfunction of a relapsing-remitting nature. It typically emerges within 3 months of COVID-19 infection and lasts at least 12 weeks.
Commonly reported symptoms include a new onset of neuropsychiatric impairment (eg, “brain fog,” memory and attentional issues), dysautonomia, depression and/or anxiety, post exertional malaise (PEM), hair loss, and musculoskeletal pain.1
Not only has long COVID proven to be an often disabling condition precluding many from returning to full-time work, it also disproportionately affects minorities and those who have historically been marginalized in health care settings.2 Specifically, the Centers for Disease Control and Prevention (CDC) reports that women, Hispanics, and bisexual and transgender adults are more likely to be diagnosed with long COVID than their respective counterparts.3
This is particularly problematic for many reasons, not the least of which is the tremendous economic burden accompanying long COVID. Ultimately, the totality of the lived experience of having long COVID carries with it an exorbitant toll in which all aspects of one’s life—including mental health—is negatively affected.4
As of this writing, there are no objective tests or biomarkers to determine a diagnosis of long COVID. Many of the symptoms themselves are subjective in nature, further complicating diagnostic clarity. This may be one of the reasons discrimination and stigmatization of this invisible illness is so rampant according to recent studies.
In one such study, 95% of respondents reported experiencing stigma related to their long COVID condition. More than 60% felt compelled to be cautious about whom to disclose their illness to, and 34% of those who disclosed their condition regretted having done so due to the response they received.5
Epistemic Injustice Common for Long-Haulers
It might be reasonable to expect the sources of such discrimination to have been family members, friends, and coworkers. This is certainly the case and, anecdotally, there are numerous accounts from long-haulers of rampant criticism, lack of support, and accusations of illness feigning.
Even a cursory review of long COVID support group forum boards revealed countless cases of families being torn apart because of long COVID stigma.6 It is no wonder, then, that so many long-haulers describe feeling isolated, ostracized, and abandoned by the very individuals they want to rely on the most.
As hurtful as it is for loved ones to not believe, it can be dangerous when medical professionals dismiss long-haulers’ symptoms and concerns. This in turn compromises an individual’s engagement in health-promotive behaviors and contributes to poorer health outcomes, depression, and lower quality of life.7
Examination of the negative interactions long-haulers experience with their medical providers reveals 2 significant trends: lack of understanding of long COVID and/or dismissal of long-haulers’ concerns. Unfortunately, what many long-haulers find is that they are now newcomers to a long line of medical stigmatization that has historically included HIV, chronic fatigue syndrome, Lyme disease, fibromyalgia, and lupus (Table).
Table. Key Concepts Defined
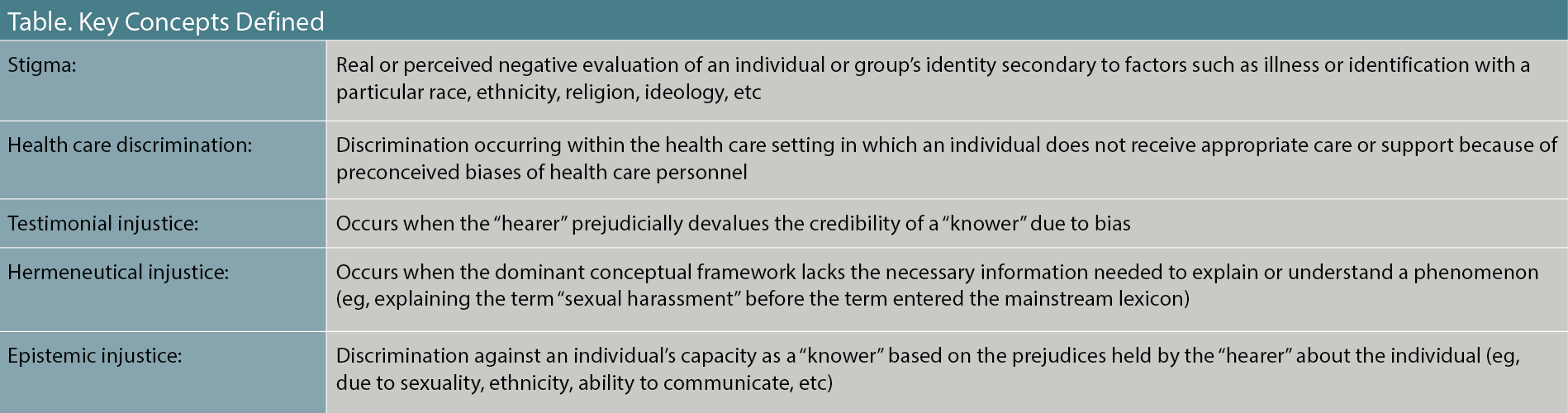
Clinicians are ethically obligated to reflect on how implicit and explicit biases may impact health care. One framework of doing so is by considering how epistemic injustice affects their patients.
As conceptualized by Fricker,8 there are 2 broad types of epistemic injustice: testimonial and hermeneutical. Each of these contributes to an individual (the “knower”) being undermined in their attempts to share their knowledge (“testifying”) to another person (the “hearer”). At the most fundamental level, the hearer discounts or rejects the knower’s credibility, often due to prejudicial bias.
Testimonial injustice reflects the type of discrimination so commonly described by long-haulers—specifically, that their individual lived experiences are discounted because of clinicians’ implicit or explicit biases toward the group to which the individual belongs, thus causing a “credibility deficit.” Common victims of testimonial injustice include psychiatric patients, women, minorities, and those with chronic and/or invisible illnesses.9
In contrast, hermeneutical injustice occurs when an individual’s lived experience is not well understood by others and even potentially by the individual themselves because those experiences do not neatly fit into existing frameworks.
Essentially, this form of injustice refers to the ability to understand (“interpret”) and/or communicate lived experience effectively. Barriers to understanding may be inadvertent (as in the case of a patient who does not know how to describe their symptoms) or willful (eg, a clinician’s ignorance of a condition that is not actively corrected).
One example of hermeneutical injustice occurs when a patient, lacking a clear way to articulate their symptoms, may express themselves more emotionally or utilize lay terms. This in turn may compromise a clinician’s ability to make sense of the patient’s experience because biomedicine tends to put greater value on scientific and/or objective data than on the patient’s experiential knowledge.9-11 Unfortunately, as Fricker so aptly notes, such “hermeneutical lacunas are like holes in the ozone: It’s the people who live under them that get burned.”8
For years, studies have consistently shown the rampant epistemic injustices experienced by those with chronic fatigue syndrome, fibromyalgia, and chronic pain. In the case of long COVID, research clearly demonstrates the link between such epistemic injustice and stress, depression, anxiety, and health-related quality of life.4,12
For long-haulers, epistemic injustice also places a disproportionate burden on them to find clinicians who will even believe their symptoms are real, much less be knowledgeable enough about the condition to provide adequate health care.6,13
Case Vignette
“Sarah” is a 36-year-old mildly overweight African American woman who works as a labor and delivery nurse at a prominent hospital in Boise, Idaho. She originally contracted COVID-19 in February 2021. Her predominant symptoms included loss of smell, GI complaints, and extreme fatigue. She did not require medical intervention, and the infection ran its course within 2 weeks. She did not experience any lingering post-viral symptoms except for continuation of anosmia.
Sarah contracted COVID-19 a second time in January 2022 despite being vaccinated. Within a week of her infection, she was admitted to the ICU with a 101○F fever and an SpO2% of 67. She remained in the ICU and on supplemental oxygen for 14 days. During that time, she was provided pulmonary therapy and treatment for a blood clot. Upon discharge, she remained on supplemental oxygen for 3 months before finally improving enough to rely on her prescription inhaler.
Around this time Sarah realized that she still had not fully recovered from her illness. She continued to experience debilitating fatigue and developed new onset of myalgia, nausea, and cognitive impairment (eg, inability to sustain attention, word finding difficulties, and short-term memory deficits).
Seeking help from her primary care manager (PCM), Sarah told him, “The exhaustion is overwhelming, like a tidal wave coming over me that I can see but can’t escape. I can’t remember what my kids told me just 10 minutes ago, much less what I did yesterday.” Lab work showed only a vitamin D deficiency. Her PCM directed Sarah to return to work despite her concerns and suggested that her fatigue was due to deconditioning secondary to having been bedridden.
Sarah knew she was not fit to take care of patients, so she remained on FMLA. She tried to resume exercise, but found this to be impossible. Even walking for 30 minutes led to her “crashing” and unable to function. Nothing seemed to help her new musculoskeletal pain or her “brain fog.” She returned to her PCM, frustrated that she was still unable to work and increasingly depressed because she was not able to contribute to her family as she once did. The front desk had her complete a PHQ-9, and her responses indicated moderately severe depression.
As Sarah began describing her cognitive challenges, her PCM interrupted her, explaining that this was likely due to poor sleep and depression. He recommended a selective serotonin reuptake inhibitor (SSRI), ignoring her protestations that most of the problems she positively endorsed on the PHQ-9 were related to the physical symptoms she was describing.
“I’m a nurse, and I know myself. This isn’t just in my head.” Ultimately, Sarah left her doctor’s office feeling defeated and helpless. She knew she was not imagining how bad she felt, but her PCM certainly made her question her own sanity. Sarah felt lost and like a shell of her former self. No one—not even her PCM—believed her or understood just how awful she felt.
When Sarah arrived home, her husband, “Taylor,” asked how her appointment went. After she told him what had happened, she saw the annoyance and hostility on his face. “I’m sick and tired of this,” he said. “Even your doctor thinks it’s all in your head. It’s time for you to just get on with it. I can’t keep doing everything to keep our family going.”
Dismantling Epistemic Injustice as a Health Care Professional
Epistemic injustice remains an integral component of social injustice, exacerbating adverse multigenerational population health outcomes in the form of health care distrust, decreased socioeconomic potential, psychological stress, trauma, and poor health.14 Although there ideally would be a societal shift in how invisible illnesses like long COVID are perceived, it is imperative that health care clinicians be advocates for change and minimize the barriers to care so inherent to epistemic injustice.
To that end, clinicians must recognize and acknowledge the injustices experienced by long-haulers who all too often report feeling marginalized and helpless. Medical professionals should also listen to their patients from a place of humility that fosters mutual understanding and improved collaboration. Finally, as advocated by Pot, clinicians should engage in “epistemic solidarity” (eg, actively supporting others as credible knowers).11
Dr Henderson is a staff clinical psychologist at the Washington Anxiety Center of Capitol Hill.
References
1. Davis HE, McCorkell L, Vogel JM, Topol EJ. Author correction: Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(6):408.
2. Suran M. Long COVID linked with unemployment in new analysis. JAMA. 2023;329(9):701-702.
3. National Center for Health Statistics. US Census Bureau, Household Pulse Survey, 2022-2023. Long COVID. Reviewed August 16, 2023. Accessed August 20, 2023. https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm
4. Samper-Pardo M, Oliván-Blázquez B, Magallón-Botaya R, et al. The emotional well-being of long COVID patients in relation to their symptoms, social support and stigmatization in social and health services: a qualitative study. BMC Psychiatry. 2023;23(1):68.
5. Pantelic M, Ziauddeen N, Boyes M, et al. Long covid stigma: Estimating burden and validating scale in a UK-based sample. PLoS One. 2022;17(11):e0277317.
6. Lewis-Jackson S, Ziebland S. Long covid, like most chronic illness, is having a dramatic effect on family life, schooling, and relationships. University of Oxford Medical Sciences Division. September 8, 2022. Accessed August 20, 2023. https://www.phc.ox.ac.uk/news/blog/long-covid-like-most-chronic-illness-is-having-a-dramatic-effect-on-family-life-schooling-and-relationships-1
7. Scholz U, Bierbauer W, Lüscher J. Social stigma, mental health, stress, and health-related quality of life in people with long COVID. Int J Environ Res Public Health. 2023;20(5):3927.
8. Fricker M. Epistemic Injustice: Power and the Ethics of Knowing. Oxford University Press; 2007.
9. Crichton P, Carel H, Kidd IJ. Epistemic injustice in psychiatry. BJPsych Bull. 2017;41(2):65-70.
10. Kidd IJ, Carel H. Epistemic injustice and illness. J Appl Philos. 2017;34(2):172-190.
11. Pot M. Epistemic solidarity in medicine and healthcare. Med Health Care Philos. 2022;25(4):681-692.
12. Kingstone T, Taylor AK, O’Donnell CA, et al. Finding the ‘right’ GP: a qualitative study of the experiences of people with long-COVID. BJGP Open. 2020;4(5):bjgpopen20X101143.
13. Au L, Capotescu C, Eyal G, Finestone G. Long covid and medical gaslighting: dismissal, delayed diagnosis, and deferred treatment. SSM Qual Res Health. 2022;2:100167.
14. Stangl AL, Earnshaw VA, Logie CH, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31.

